Quality Healthcare
American Indians and Alaska Natives have long struggled to obtain and access quality healthcare, despite the fact that the federal government’s trust agreements with Native governments included providing healthcare services for American Indian and Alaska Native communities. Though the first federal appropriations for Native healthcare occurred more than 180 years ago, the pace of change from the healthcare system of the past to one which delivers truly quality care consistently to all American Indians and Alaska Natives has been frustratingly slow.
During their lifetime, elders have likely experienced poor services, barriers to access and outright discrimination when trying to access healthcare. However, the new millennium brought a push to improve healthcare systems and recent legislation has reshaped the way healthcare is delivered to all people in the United States. American Indian and Alaska Native elders stand to benefit from these changes which seek to create “quality” healthcare for all.
While “quality” healthcare sounds simple, there are six different aspects to healthcare delivery that determine the quality of the care itself and the value to patients in the end. The Institute of Medicine developed six “aims for improvement” to healthcare in 2001, and they have greatly influenced the direction of healthcare improvement in the U.S. These aims are safety, effectiveness, efficiency, equitability, timeliness and patient-centered focus. A patient-centered focus ensures that the patient is treated with care and consideration for cultural differences and their own unique healthcare needs. It ensures that medical professionals help patients understand their condition, the available care options and respect the patient’s health care choices.
Creating a Welcoming Facility for Elders
Service providers face a variety of challenges in meeting the needs of the aging population. One of these challenges is creating service delivery systems which consider the needs of a diverse population. Currently, American Indian and Alaska Native elders are often overlooked and underserved. This is partially due to the lack of understanding of where they access services, but because many services available to American Indians and Alaska Natives have not been culturally competent in their delivery of care. Additionally, many urban programs fail to meet the unique cultural needs of Native elder populations. An understanding of their belief systems can enable healthcare providers to more effectively and respectfully interact Native elders.
 Recognition
Recognition
With some 78 percent of American Indians and Alaska Natives living outside of Indian lands, the need to recognize Native people in facilities both on and outside of tribal areas is increasingly important. This can be a challenge because it is not always obvious or readily apparent that a person identifies as Native. Without recognizing an elder as American Indian or Alaska Native, it is not possible to understand the differing worldviews they might have, or the adversities they’ve faced throughout history (such as racism and the many destructive U.S. Indian policies). It is important to note that beliefs are not homogenous among Native elders, as some may have traditional views and others may not. There are 574 federally recognized tribes and more awaiting federal recognition. Language, beliefs and practices vary widely among these groups.
Involvement
The Health Resources and Services Administration (HRSA) advised that the delivery of culturally competent care requires understanding of the patient’s healthcare literacy. This is influenced by such factors as education and income, but for Native elders it may more seriously be impacted by historical inequities in access to healthcare services and disparities in treatment. The HRSA also recommends the assessment of relevant cultural factors that might impact the patient’s health. For Native elders, language and traditional practices are important cultural factors to consider alongside the many other aspects of diversity.
Care that is culturally competent requires the inclusion and participation of the care recipient. It is not always possible to truly provide quality care to an elder without understanding who they are and where they come from. To ensure willing participation from an elder, their family and their community in delivering any type of service, whether institutional or home and community based, the involvement of the entire community in the development and delivery of care is critical. Involvement on a community level can help to identify the needs specific to the Native population served by your facility. The needs of American Indian and Alaska Native populations vary in terms of the specific beliefs and care preferences and it is important for service providers to fully understand those needs and not make assumptions.
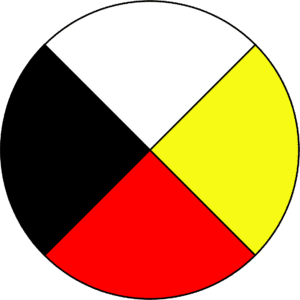 While the specific beliefs of each Native nation vary and may be specific to that nation alone, there are some broader shared beliefs that apply to many. With regard to healthcare, the “Medicine Wheel” or “Sacred Hoop” is used by many for health and healing purposes. The Medicine Wheel contains four directions: north, east, south and west. For tribes, the directions have different meanings. It may represent the seasons of the year, the stages of life or aspects of life, but is always used to reflect a more holistic view toward life.
While the specific beliefs of each Native nation vary and may be specific to that nation alone, there are some broader shared beliefs that apply to many. With regard to healthcare, the “Medicine Wheel” or “Sacred Hoop” is used by many for health and healing purposes. The Medicine Wheel contains four directions: north, east, south and west. For tribes, the directions have different meanings. It may represent the seasons of the year, the stages of life or aspects of life, but is always used to reflect a more holistic view toward life.
American Indians and Alaska Natives understand that people are interconnected to their communities, to nature and to the spiritual world. When confronting an ailment, it may be viewed as a lack of harmony between the physical body and the mind, spirit and emotions of a person. Accordingly, many Native people may choose to look towards western medicine to address the symptoms of an ailment while also pursuing spiritual guidance from traditional healers in their communities to recover from an imbalance between the mind, soul and body.
Traditional healers utilize medicinal plants and herbs as well as sacred ceremonial practices such as sandpainting or sweat lodges to help correct such imbalances in the patient-seeking treatment. Since the introduction of western medicine to Native communities, traditional practices have often been viewed as at odds with Western medical practices. Historical oppression and motives to force the assimilation of American Indians and Alaska Natives into the broader melting pot of the U.S. have resulted in little consideration or deference for such traditions.
Taking Action
Listening to the community and specific individuals in the service delivery system is as important as developing programs specific to American Indian and Alaska Native needs. The historical neglect of the unique needs of Native people in the broader healthcare system has meant that many elders have experienced poor-quality healthcare and may not be willing to trust a care provider that promises to hear their concerns but fails to act.
Taking inclusive action means including American Indians and Alaska Natives in the delivery of care. Members of a Native elder’s community may be able to assist with the unique needs in a culturally sensitive way that would otherwise not be possible for non-Natives. Hiring qualified American Indians and Alaska Natives as staff and into administrative positions can lend a shared perspective between those designing, giving and receiving care as well as create trust on an individual and community level.
Inclusivity can be demonstrated in a number of ways. One is by featuring Native people in promotional and marketing materials. Recognizing traditional holidays and feast days and participating in Native community events can help to create understanding, as will learning the appropriate ways to show respect toward elders. Repeated efforts to reach out will help create a relationship of trust over time.
Better healthcare outcomes for Native elders depends upon more than just providing the best medicine. With a better understanding of and respect for the whole individual — including their American Indian and Alaska Native culture, beliefs and practices — better healthcare outcomes can be achieved.
 Storytelling in Patient-Centered Native Healthcare
Storytelling in Patient-Centered Native Healthcare
Storytelling is as much about education as it is about entertainment. It is through storytelling that each tribe’s history and cultural traditions are passed down from one generation to the next.
Stories not only reflect knowledge of communities, they also highlight core values that are important to tribal society. They offer tribes an auditory record of their traditional spirituality and history and can be a valuable tool for emphasizing health and wellness.
Sharing stories is a major consideration for providing health care at the Southcentral Foundation, which offers health services to American Indian and Alaska Native people in southcentral Alaska. The Southcentral Foundation bases its services on a foundation of trust between care providers and patients.
Through storytelling, providers and patients can build relationships while honoring tribal traditions. These stories can be utilized to help motivate tribal members to readopt healthy lifestyles and practices that were traditionally part of their culture.
Southcentral Foundation integrated culture and storytelling and forever changed the Alaska Native health care system. Learn how they use culture and storytelling in healthcare to treat the whole person. A short video from the Southcentral Foundation describes the role of storytelling in their care model and offers examples of its positive effects on health outcomes.